If you’re searching for dental implant cost in London, chances are you’re seriously considering treatment — and want clear, honest answers before booking.
Dental implants are a long-term investment in your smile, comfort, and confidence. In this guide, we’ll break down how much dental implants cost in London, what affects the price, and how to decide if implants are right for you.
How Much Do Dental Implants Cost in London?
In London, the average cost of a single dental implant typically ranges from:
£2,000 – £3,500 per tooth
This usually includes:
- Implant (titanium screw)
- Abutment (connector)
- Final crown (visible tooth)
- Surgical placement
- Follow-up appointments
Be cautious of very low prices — implants are a precision treatment, and quality materials and expertise matter.
What Affects the Cost of Dental Implants?
There isn’t a one-size-fits-all price. Several factors influence the final cost:
1. Number of Implants Needed
Replacing one tooth costs less than replacing multiple teeth or a full arch.
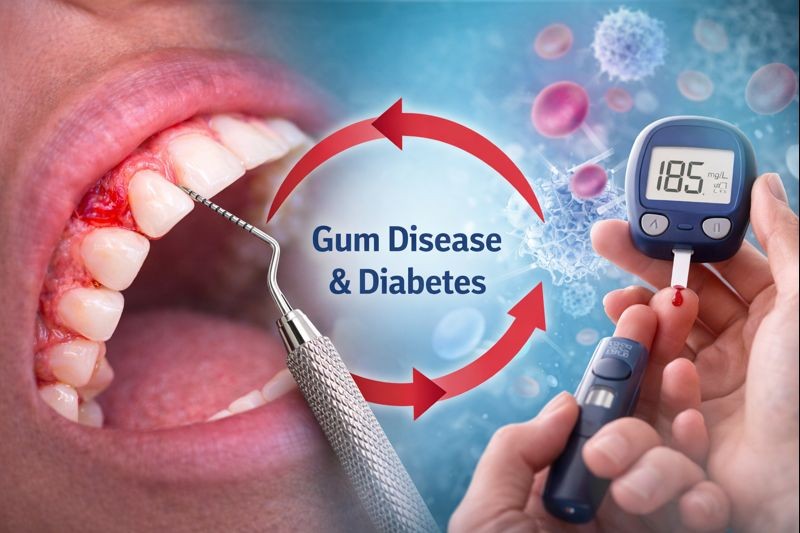
2. Bone Density & Preparation
Some patients require:
- Bone grafting
- Sinus lift procedures
These add complexity — and cost — but improve long-term success.
3. Implant Brand & Materials
High-quality, well-researched implant systems cost more but offer:
- Better integration
- Higher success rates
- Longer lifespan
4. Experience of the Implant Dentist
Expert planning and surgical skill reduce complications and improve outcomes — an important factor when choosing where to book.
Are Dental Implants Worth the Cost?
For many patients, yes — absolutely.
Compared to bridges or dentures, dental implants:
- Last significantly longer
- Protect jawbone health
- Look and feel like natural teeth
- Don’t rely on neighbouring teeth for support
While the upfront cost is higher, implants often prove more cost-effective long term.
Why Dental Implant Prices Vary Across London
If you’ve searched “implants near me”, you’ll notice prices vary widely.
This is often due to:
- Clinic location and overheads
- Technology used (3D scans, digital planning)
- Length of aftercare and follow-up
- Whether treatment is done by a general dentist or implant specialist
Always compare what’s included, not just the headline price.
Can I Spread the Cost of Dental Implants?
Many London clinics offer payment plans or finance options to make implants more affordable.
This allows you to:
- Spread the cost monthly
- Start treatment sooner
- Avoid compromising on quality
Ask about flexible payment options during your consultation.
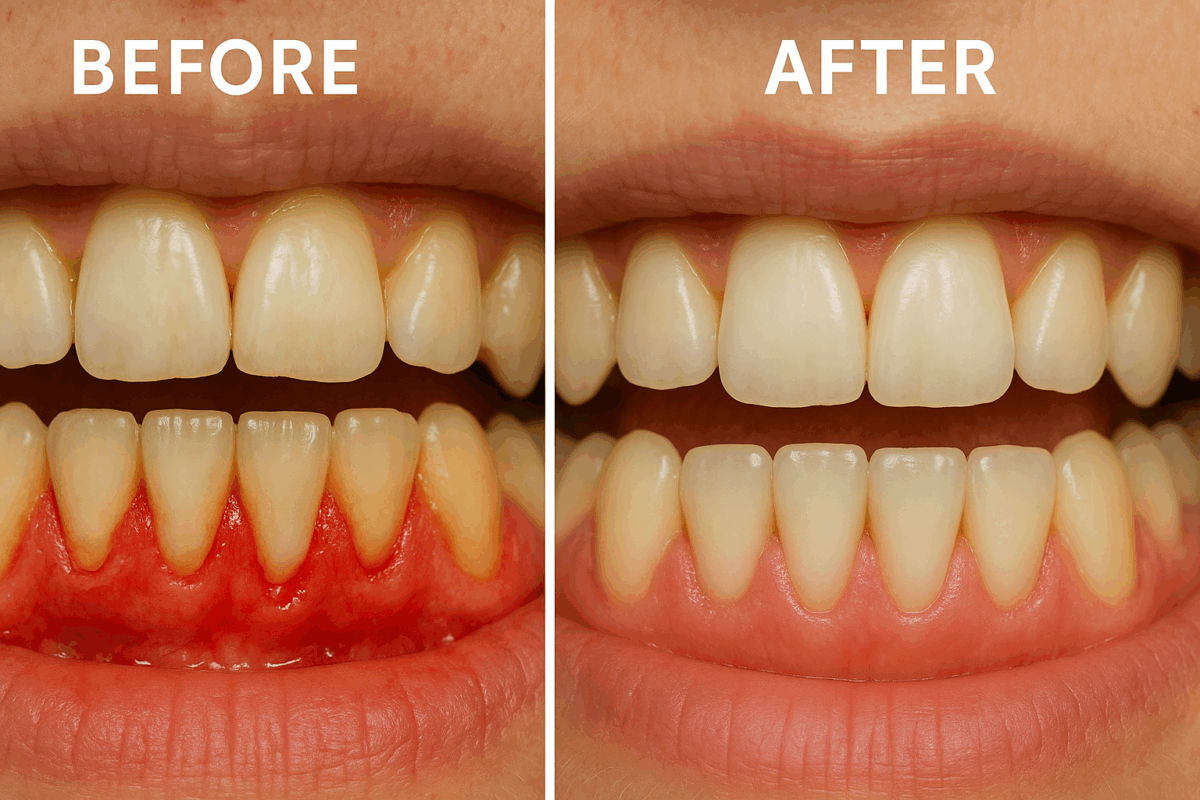
What’s Included in a Dental Implant Consultation?
A proper implant consultation usually includes:
- Full oral examination
- 3D imaging or X-rays
- Assessment of bone and gum health
- Personalised treatment plan
- Transparent cost breakdown
This is the best way to get an accurate price — not just an online estimate.
Looking for Dental Implants Near You in London?
If you’re ready to move forward, the next step is simple.
– Get expert advice
– Understand your exact costs
– Explore your treatment options
– Ask questions — with no pressure
Book a dental implant consultation today and find out exactly how much your treatment would cost.
Ready to Book?
Dental implants are a long-term solution — choosing the right team matters.
Speak to an experienced implant dentist and take the first step towards a confident, complete smile.