Gum Disease and Diabetes: The Science Behind the Link
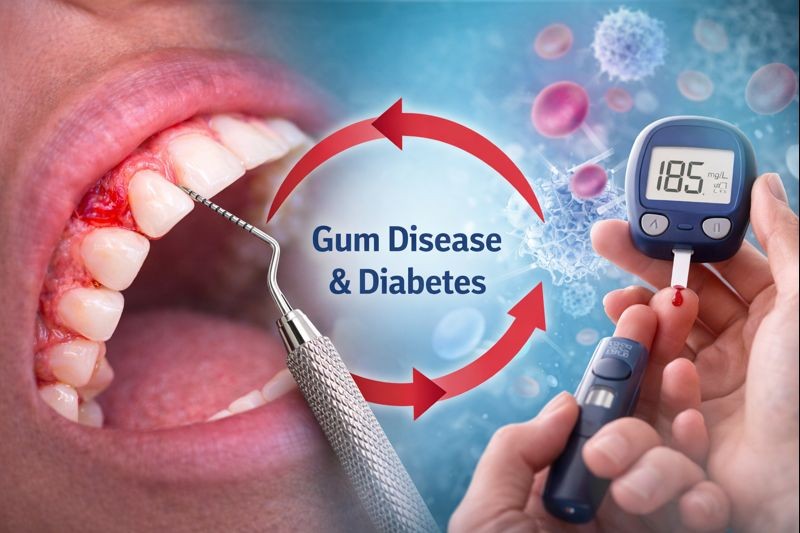
Gum disease and diabetes are closely connected through inflammation, immunity, and blood sugar control. This relationship is so well established that gum disease is now considered the sixth complication of diabetes by medical professionals.
At Hammersmith Dental Care, we regularly support patients with diabetes by providing specialist periodontal care designed to protect both oral and general health.
What Is Gum Disease?
Gum disease, also called periodontal disease, is a chronic inflammatory condition caused by harmful bacteria living below the gumline.
It develops in stages:
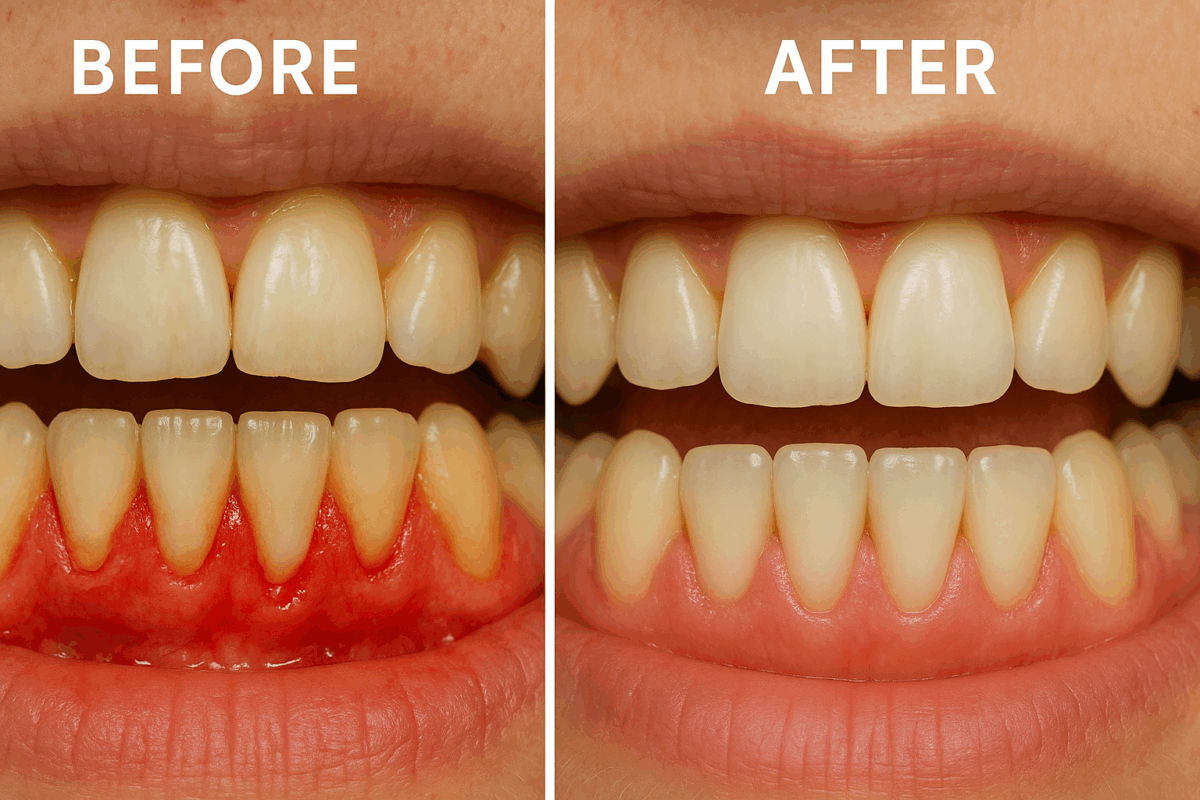
🔹 Gingivitis
- Caused by plaque bacteria irritating the gums
- Leads to redness, swelling, and bleeding
- Reversible with professional care
🔹 Periodontitis
- Occurs when inflammation spreads deeper
- The immune system begins to damage bone and tissue
- Results in gum recession, bone loss, and loose teeth
- Not reversible, but can be stabilised
The key driver is chronic inflammation, which plays a major role in its link with diabetes.
What Is Diabetes? (And Why It Affects Healing)
Diabetes affects how the body regulates blood glucose (sugar). When blood sugar levels remain high:
- White blood cells become less effective
- Inflammation increases throughout the body
- Healing slows down
- Infection risk rises
This makes people with diabetes more vulnerable to infections, including infections of the gums.
The Science: How Diabetes Makes Gum Disease Worse
From a biological perspective, diabetes impacts gum health in several ways:
- Impaired Immune Response
High blood sugar weakens the immune system, making it harder to fight the bacteria responsible for gum disease.
- Increased Inflammation
Diabetes increases inflammatory markers in the bloodstream. In the gums, this leads to:
- Faster tissue breakdown
- Greater bone loss
- More severe periodontitis
- Reduced Blood Flow
Diabetes affects small blood vessels, limiting oxygen and nutrient delivery to the gums — slowing healing after infection or dental treatment.
The Reverse Effect: How Gum Disease Affects Blood Sugar
Gum disease doesn’t stay in the mouth.
The bacteria and inflammation associated with periodontitis:
- Enter the bloodstream
- Increase systemic inflammation
- Interfere with insulin function
What the Science Shows
Multiple studies confirm that untreated gum disease makes blood sugar levels harder to control, while periodontal treatment can lead to measurable improvements in HbA1c levels (a key diabetes marker).
In simple terms:
Healthy gums help support better diabetes control.
Warning Signs Diabetic Patients Should Never Ignore
People with diabetes should be especially alert to:
- Bleeding gums
- Red, swollen, or tender gums
- Persistent bad breath
- Gum recession
- Teeth that feel loose
- Slow healing after dental work
Because gum disease can be painless, regular checks are essential.
Why Periodontal Treatment Is Especially Important for Diabetics
Without treatment, gum disease can lead to:
- Accelerated bone loss
- Tooth loss
- Implant complications
- Increased systemic inflammation
- Poor diabetes control
Early periodontal care reduces bacterial load and inflammation — benefiting both oral and general health.
Periodontal Treatment for Diabetic Patients at Hammersmith Dental Care
At Hammersmith Dental Care, our approach is evidence-based and tailored to patients with diabetes:
- Detailed gum assessments
- Deep cleaning (scaling and root planing)
- Careful infection control
- Supportive periodontal maintenance
- Long-term prevention strategies
We focus on stabilising gum health while supporting overall wellbeing.
Practical Steps Diabetic Patients Can Take to Protect Their Gums
✔ Maintain stable blood sugar levels
✔ Brush twice daily with fluoride toothpaste
✔ Clean between teeth every day
✔ Attend regular hygiene appointments
✔ Seek early periodontal assessment
✔ Avoid smoking or vaping
Prevention and early intervention are key.
When Should a Diabetic Patient See a Periodontist?
You should book a periodontal assessment if:
- You have diabetes and bleeding gums
- Gum disease keeps returning
- You notice gum recession
- You have loose teeth or implants
- You want to reduce long-term health risks
Specialist care leads to better outcomes.
References
- NHS – Gum Disease: https://www.nhs.uk/conditions/gum-disease/
- NHS – Diabetes: https://www.nhs.uk/conditions/diabetes/
- British Society of Periodontology – Systemic Health: https://www.bsperio.org.uk
- American Academy of Periodontology – Diabetes & Gum Disease: https://www.perio.org/consumer/diabetes-and-periodontal-disease
- Preshaw PM et al., Periodontitis and Diabetes: A Two-Way Relationship, Diabetologia