Gum disease doesn’t happen overnight. It develops gradually — often silently — starting with plaque build-up and potentially progressing to serious bone damage.
Understanding how gum disease starts, the link between plaque and gum disease, and the risk of bone loss from gum disease can help you protect your long-term oral health.
This guide explains the science behind each stage — and why early treatment matters.
Stage 1: Plaque Build-Up – The Beginning of Gum Disease
If you’re wondering how gum disease starts, the answer is plaque.
Plaque is a sticky bacterial biofilm that forms on teeth daily. When it isn’t removed through proper brushing and interdental cleaning:
- Bacteria multiply rapidly
- Toxins irritate the gum tissue
- Inflammation begins at the gumline
At this early stage, the condition is still reversible.
Stage 2: Gingivitis – Early Gum Inflammation
Persistent plaque leads to gingivitis, the first stage of gum disease.
Symptoms include:
- Bleeding when brushing or flossing
- Red or swollen gums
- Mild tenderness
- Bad breath
Importantly, gingivitis does not cause bone damage and can be reversed with professional cleaning and improved home care.
Read more in our internal guide: Why are my Gums bleeding .
Stage 3: Periodontitis – When Infection Spreads Below the Gums
If gingivitis is left untreated, bacteria spread below the gumline.
This stage is called periodontitis, and it marks the transition from inflammation to structural damage.
During periodontitis:
- Gums detach from teeth
- Periodontal pockets form
- Infection progresses deeper
- Tissue begins breaking down
This is where plaque and gum disease become significantly more destructive.
Stage 4: Bone Loss from Gum Disease
One of the most serious consequences of untreated periodontitis is bone loss from gum disease.
Here’s how it happens:
- Bacterial infection triggers chronic inflammation
- The immune response damages supporting tissues
- The jawbone surrounding the teeth begins to deteriorate
- Teeth loosen and may eventually fall out
Bone loss is irreversible without advanced intervention — which is why early diagnosis is critical.
The Scientific Link Between Plaque and Gum Disease
The relationship between plaque and gum disease is well-established in dental research.
Plaque bacteria release toxins that:
- Stimulate inflammatory chemicals
- Destroy connective tissue fibres
- Activate bone resorption (bone breakdown)
If plaque hardens into tartar (calculus), it cannot be removed at home and requires professional hygiene treatment.
Risk Factors That Accelerate Progression
You may be at higher risk of developing advanced gum disease if you:
- Smoke or vape
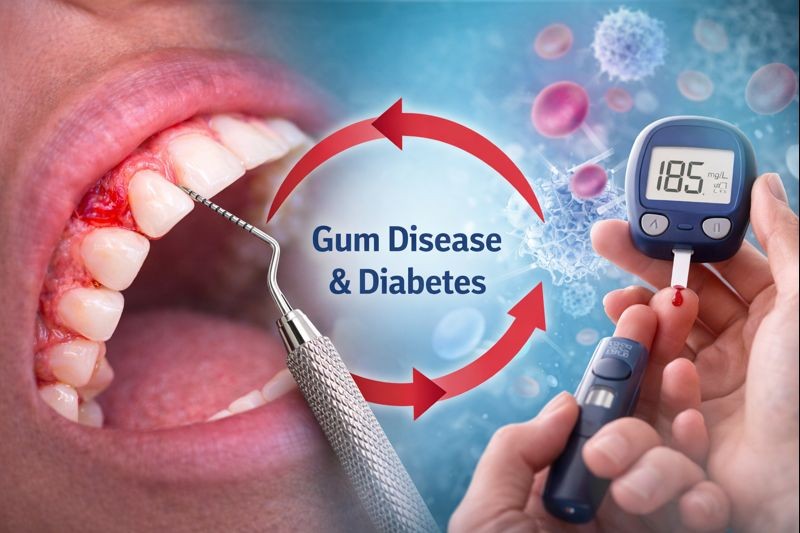
- Have diabetes
- Miss regular hygiene visits
- Have a genetic predisposition
- Experience chronic stress
Even patients who brush regularly can develop gum disease if interdental cleaning is inadequate.
How to Prevent Gum Disease and Bone Loss
Stopping gum disease early prevents permanent damage.
Daily Prevention
- Brush twice daily with fluoride toothpaste
- Clean between teeth using floss or interdental brushes
- Attend regular hygiene appointments
Professional Treatment
If pockets or bone loss are detected, periodontal treatment may include:
- Deep cleaning (root surface debridement)
- Targeted antibacterial therapy
- Ongoing maintenance care
Visit our Gum Disease Treatment pillar page to learn about all available options.
Key Takeaway: Early Action Prevents Bone Loss
To summarise:
- Plaque forms daily
- Gum inflammation begins quietly
- Infection spreads below the gumline
- Bone loss from gum disease can occur without pain
Understanding how gum disease starts allows you to intervene early — before permanent damage occurs.
Concerned About Bleeding or Swollen Gums?
Don’t wait for symptoms to worsen.
Book a professional gum health assessment today and protect your teeth — and the bone that supports them — for the future.
Early treatment is always simpler, less invasive, and more predictable.